The evolution of in vitro fertilization has been tremendous in the last few decades. Technological innovation has made what was once viewed as a complicated and unpredictable process much more accurate and efficient. State of the art IVF centres are now dependent on the latest tools to enhance diagnosis, embryo quality and success rates. For couples seeking treatment, a clear and assuring explanation of how technology can help in IVF can be helpful. When visiting an ivf centre near me, many patients are surprised to learn how deeply technology influences every step of the fertility journey.
Highly sensitive blood tests are used in modern IVF centres to check the major reproductive hormones which include AMH, FSH, LH, estrogen and progesterone. These indicators can be used to evaluate ovarian reserve, ovulation, and hormonal balance. Proper hormonal profiling enables the fertility experts to tailor the stimulation regimes, enhance the egg quality results, and minimize the chances of overstimulation in the IVF cycles.
High-quality ultrasound offers extensive images of ovaries, follicles, uterus, and endometrial lining. 3D imaging can detect any abnormalities in the uterus like fibroids, polyps or structural anomalies that can influence the implantation. The use of high-resolution scans regularly provides accurate timing of egg retrieval and embryo transfer to improve the success rate of IVF.
Preimplantation genetic testing enables embryologists to check embryos on chromosomal abnormalities prior to transfer. The technology assists in the detection of healthy embryos with the best implantation chances and minimizing the risk of miscarriage. Genetic screening is particularly beneficial to couples experiencing frequent pregnancy loss, maternal age, or genetically inherited disorders, enhancing safety and results.
Modern semen analysis is not just about sperm count and motility. Sperm DNA fragmentation, morphology and functional integrity are now assessed by technologies. Such insights assist doctors to choose the best method of fertilization and prescribe treatment to enhance the quality of sperm. Proper diagnosis is crucial in the treatment of male factor infertility in IVF.
Time-lapse incubators are used to take constant pictures of growing embryos, without taking them out of controlled conditions. The technology enables the embryologists to view the growth patterns, time of cell division, and embryo behavior. Constant observation enhances accuracy of embryo selection and reduces stress associated with environmental alteration resulting in improved implantation potential.
The modern incubators replicate the conditions within the human body closely by regulating the temperature, oxygen levels, humidity, and pH levels to the optimal levels. These controlled conditions help to develop healthier embryos and alleviate external stress. Good incubation conditions are essential in enhancing the quality of the embryo and the chances of successful pregnancy.
IVF labs have sophisticated air filters to ensure that the environment is sterile and free of contaminants. Embryo can be influenced by even the slightest exposure to toxins, chemicals or changes in air quality. The use of high-efficiency filtration guarantees uniformity, embryo protection, and stable laboratory conditions that are crucial to the attainment of stable IVF results.
Digital tracking systems are used in modern IVF labs to track embryos, samples and patient data with high accuracy. Automated labeling and monitoring saves on human error and enhances safety. Digital records can also enable fertility teams to understand trends, streamline lab operations, and keep transparency during the IVF process.
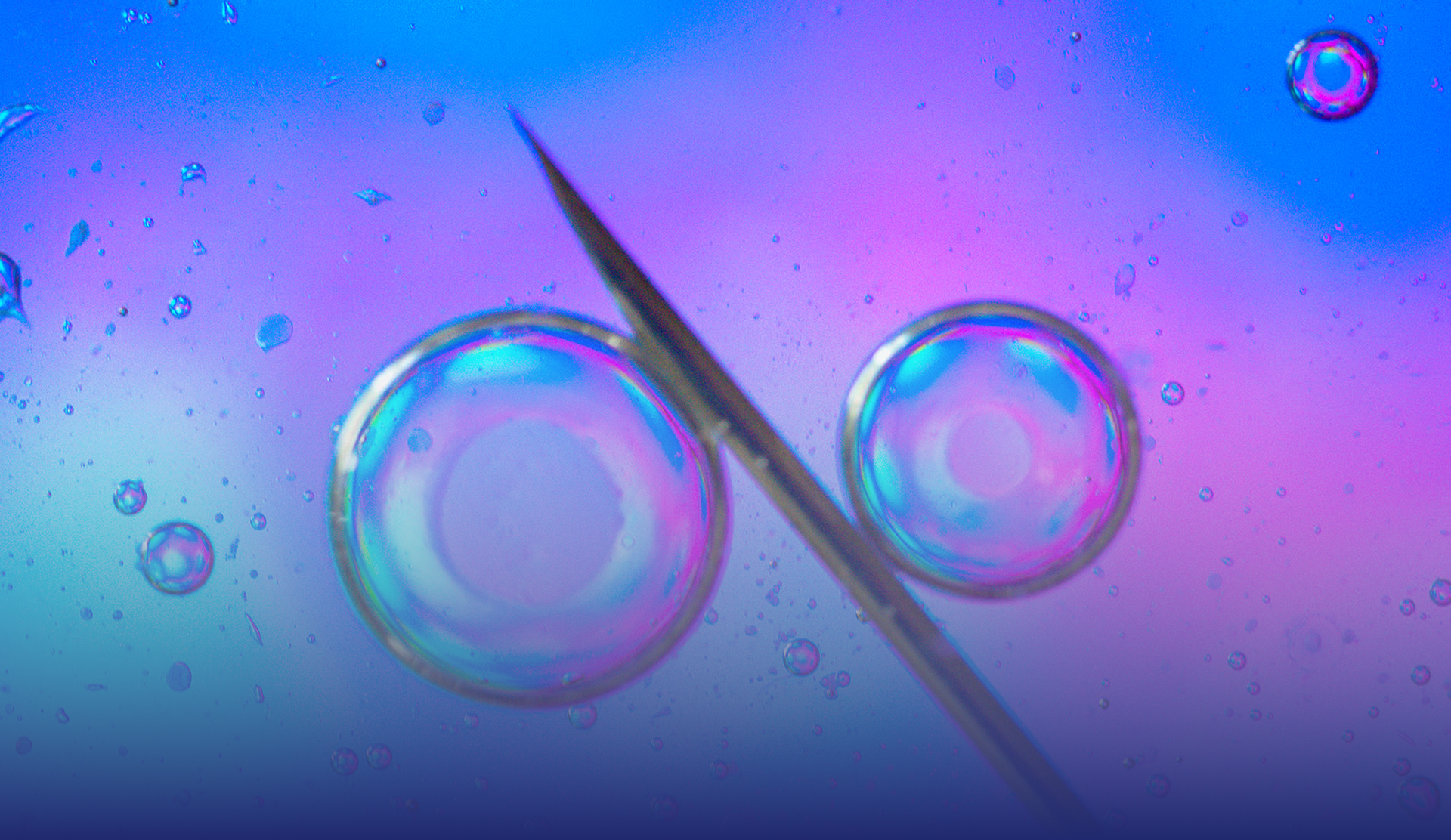
ICSI is the procedure of fertilizing an egg by injecting a single healthy sperm. The method is particularly useful in cases of severe male infertility such as low sperm count or poor motility. ICSI has a huge success rate in enhancing fertilization and is extensively applied where traditional methods of fertilization have failed or are not reliable.
PICSI helps to increase the selection of sperm by selecting sperm capable of binding with hyaluronic acid, which is a sign of maturity and DNA integrity. This method enhances the quality of the embryo and minimizes the chances of genetic defects. PICSI is commonly suggested to couples with multiple IVF failures or embryo development issues in the previous cycles.
Laser-assisted hatching involves the use of laser technology to either thin or create a small hole into the outer shell of the embryo. This facilitates easier implantation of the embryo into the uterine lining. The method is especially useful in older patients, transfers of frozen embryos, or where the embryo shells are thick.
Assisted oocyte activation is used when eggs fail to fertilize despite ICSI. This technique stimulates the egg chemically or electrically to trigger natural activation processes. It is helpful in rare fertilization failure cases and can significantly improve outcomes for patients with repeated unsuccessful fertilization attempts.
Technology has transformed IVF into a more precise, personalized, and effective treatment option. Choosing a clinic that embraces modern technology can make a meaningful difference in outcomes and overall experience. When searching for an ivf centre near me, understanding the technologies they use helps you make an informed decision. As advancements continue, IVF centres will keep improving success rates and offering hope to individuals and couples on their path to parenthood.